A Steadying Force in C-Suite: The Changing Role of Biopharma CFOs
COVID-19 pandemic, the challenging capital-markets climate in biotech, and a more innovative and specialty treatment focus has increased reliance on the finance arm as a key strategic cog.
Over the past three years, the pharmaceutical industry has gone through several impactful changes. During the early months of the COVID-19 pandemic, investors flooded the industry with money, allowing new companies to emerge and conduct multiple rounds of clinical trials while still being confident that more funding would be available. Over the past year, however, things have changed and funding is harder to come by. This has put the role of chief financial officer in the spotlight.

Morgan Brown is CFO at Clene, a clinical-stage biopharmaceutical company working on treatments for neurodegenerative diseases. According to Brown, life sciences organizations are searching for new qualities in CFOs.
“Companies are looking for more contribution from the finance team on the whole, and the CFO specifically to be more strategic in nature, to really partner with the other c-suite executives and help them effectively operate the business,” he says.
Brown also elaborates on how the changing industry is impacting the role of the CFO in ways not directly connected to finance. “Although not specifically related to CFOs, I think the distribution of drugs isn’t going to be the same old retail-pharmacy model that we’ve seen in the past,” he explains. “It’s going to be more innovative and specialty pharmacy-based and at-home delivery.”
Justin Thacker, CFO at Aristea Therapeutics, says that the role has changed quite a bit over the past three years, with the past 12 months impacting the job significantly. “With the pandemic, obviously, working remotely has changed significantly for me and the teams that I’ve been involved with,” he tells Pharm Exec. “[Though] we were always moving to more automation, the pandemic pushed that along quite rapidly.”
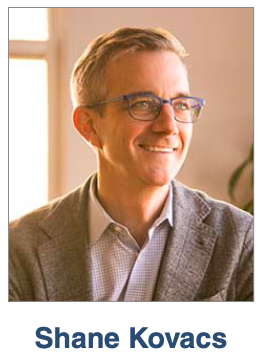
Shane Kovacs, CFO and chief operating officer at Olema Oncology, believes there’s been a “dramatic shift in the tone of the capital markets as it relates to the biotech sector.” This can have big implications for CFOs since access to capital plays a large role in the success of biotech companies, Kovacs notes, and the past decade saw one of the largest booms the biotech sector has ever seen. Unfortunately, things have changed over the past 12 months.
“[As] we have witnessed across many historical periods of enthusiastic expansion in other industries, the pendulum likely swung too far in the positive direction by early 2021,” he says. “There were many examples of new companies being formed by licensing technology and IP out of academia that then catalyzed on the relatively easy access to capital with successive private-round financings followed quickly by an IPO. Pre-money valuations for biotech IPOs that historically struggled to achieve the $200 million mark were now going public with valuations exceeding $500 million and, in some cases, greater-than-$1 billion unicorn valuations.”
Kovacs explains that these companies were able to grow very quickly due to having access to the capital.
Pharm Exec financial columnist and Editorial Advisory Board member Barbara Ryan recently described how the biotech industry peaked with investors in early 2021. The previous year, biotech and biotech IPOs provided consistently large returns for investors. Since that time, however, the biotech industry entered the longest bear market in its history, leaving many companies struggling to find further funding.
Investors are learning the difference between biotech and the tech industry, Kovacs points out. New technologies must undergo periods of trial and tribulation before being approved, and many new biotechnologies never make it to the approval stage. This creates a much longer business cycle than the tech industry and requires more capital before becoming cash-flow positive.
“Over the past 12 months, we have, unfortunately, seen a complete reversal of this investor enthusiasm for the biotech sector,” says Kovacs. “Valuations are now at all-time lows with many companies trading at or even below their cash balances. New equity offerings and IPOs have fallen off a cliff. The big question looming over the heads of biotech boards and management teams is, ‘How long will this last?’”
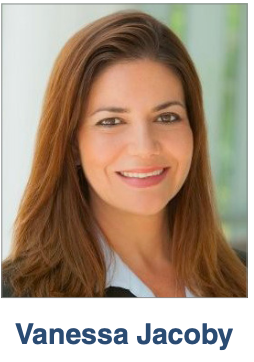
Shoreline Biosciences’ CFO, Vanessa Jacoby, notices similar trends as well.“With the volatility of the market, I think capital is becoming sparser and you have to, again, navigate the trade-offs,” she tells Pharm Exec. “What is important to your organization? How do you focus? What are the products that are more likely to make it to the clinic, and what are the unmet needs that we’re trying to solve here?”
According to Jacoby, due to the volatility of the markets, CFOs are focused on making sure that their companies are well-resourced and can deliver the goals of the wider organization. Even if the markets become less volatile, those goals will remain the same.
She adds that the pandemic likely caused a good amount of capital to flood the industry. Over the past months, however, interests have changed, and she believes that many generalist investors have moved on to different sectors.
“It’s a cyclical process,” says Jacoby. “You have a lot of resources, and then they decline, and you have to do the best that you can, always with the goal in mind to bring drugs to patients.”
BioWorld Insider Podcast: One-on-one with Medical Innovators

Another record year for biopharma financings bodes well for 2022
BioWorld Insider Podcast: One-on-one with Medical Innovators

Another record year for biopharma financings bodes well for 2022
https://www.bioworld.com/ext/resources/Podcast-files/bioworld_ep12_061221_edit2.mp3?1639088948
In another record year for biopharma fundraisings, more money than ever pulsed through the industry. The volume and value of pharma IPOs and venture capital financings are at their highest levels. Private financings for 2021 easily outdistanced those from 2020, much of it powered by SPACs. Where is it all going in 2022? Two experts joined BioWorld to share their thoughts. Kleanthis Xanthopoulos is a co-founder and executive chairman of Shoreline Biosciences. For more than 20 years he’s been an executive, company founder, CEO, investor and board member in biopharma research. Also joining the discussion was Joe Hernandez, CEO and executive chairman of Blue Water Vaccines, who founded or led eight health care and pharmaceuticals companies.
Harnessing the body’s natural killers to target cancer

Natural killer (NK) cells are part of the innate immune system, the body’s first line of defense against cancer. Credit: Alpha Tauri 3D Graphics/Shutterstock
Billions of highly trained killers are flowing through your fingers right now. They patrol your internal organs, guard the tissues under your skin against invaders, and wipe out virus-infected cells. They remain vigilant against cancer — recognising and destroying the early signs of tumours before they can gain a foothold.
These tiny terminators, called natural killer (NK) cells, are one of the body’s strongest defences against illness and disease — and yet the hundreds of billions of NK cells in our own bodies sometimes aren’t enough. Now researchers want to engineer NK cells as reinforcements, and store ranks of those reinforcement NK cells to be called up and deployed as needed (see ‘Engineering a tumor killer’). They want to make these engineered NK cells available to cancer patients and others as living drugs, without having to personalize them for each patient, as is the case with other cell therapies.
“We want to make cells that work like drugs,” says Dan Kaufman, a professor of regenerative medicine at the UC San Diego School of Medicine and co-founder and chief scientific officer of Shoreline Biosciences. “When you take a blood pressure medicine or a cholesterol medicine, everybody gets the same thing. You know the doses and it’s standardized. Using these engineered NK cells, we can do that. We can make hundreds, or potentially thousands, of doses of these NK cells all the same and use them as off-the-shelf therapies.”
Immunotherapy strategies
The idea builds on the success of so-called CAR-T cells, which are used as immunotherapies against several types of cancer. These cell-based therapies are based on a different immune component, called T cells. By collecting a patient’s T cells, engineering them to make them more potent, and then infusing them into the body, scientists can supercharge the cancer-fighting ability of the patient’s immune system. Five CAR-T cell therapies have been approved by the US Food and Drug Administration against several blood cancers.
NK cell immunotherapy has not yet reached that stage. “The natural killer cell approach in terms of cancer immunotherapy is newer, and rapidly gaining recognition,” says Hans-Gustaf Ljunggren, who works on cell therapies at the Karolinska Institute in Stockholm, Sweden. “There are numerous clinical trials going on with various natural killer cell-based products.”
Although there are clinical trials of NK cells in progress for multiple different blood cancers, nothing has been approved yet.1 “But it’s not unlikely that we will see such products within the coming five years,” Ljunggren says.
To help translate his own research on NK cells into commercial therapies, Kaufman co-founded Shoreline Biosciences. The company raised $43 million in financing earlier this year and entered into two partnerships with two immunotherapy companies, Kite Pharma and BeiGene, to develop novel cell therapies. The company recently concluded another round of financing that raised an additional $140 million.
One of the goals of NK cell therapies is to make them significantly cheaper than CAR-T cell treatments, Kaufman says. “It’s very expensive to take out the T-cells, engineer them and give them back to each individual patient. It costs roughly half a million dollars to make the cells for one patient.” The process also takes several weeks.

Innate fighters
NK cell therapies can be made more quickly and at lower cost because NK cells function in a different way. T cells are part of the adaptive immune system, the body’s second line of defence against both viral infections and cancer. They are primed to recognise specific foreign proteins on the surface of a patient’s own cells. Because T cells from one person recognize healthy cells from other people as foreign, only a patient’s own T cells can be used as a therapy — hence the need to remove and engineer them at such cost.
NK cells work in the frontline innate immune response, in which they patrol the body and attack any cells that are not recognised as part of the host tissue. This more indiscriminate approach means that NK cells therapies can be sourced elsewhere and more easily given as a standard treatment to many different patients.
“You can essentially establish banks of hopefully potent NK cells that could then be distributed globally to be used for treatment of cancers,” Ljunggren explains.
Because they do not need to be taken from a specific patient, Kaufman began developing NK cells for potential therapies from induced pluripotent stem (iPS) cells — skin or blood cells that have been reprogrammed back into an immature state that lets them develop into any other type of cell.
“Dan is one of the pioneers in the generation of the IPS derived NK cells,” Ljunggren says. “And now IPS NK cells have become a very interesting and relatively new aspect of cell therapies.”
Genetic manipulation
Besides being more universal, deriving the NK therapies from pluripotent stem cells brings another advantage. Manipulating the genome of the stem cells before they are converted to NK cells offers a reliable way to introduce genetic changes that could improve potential therapies.
When faced with attacking NK cells, cancer cell don’t sit idly by. “We know there are ways that the tumour cells can sort of evolve to avoid the immune system,” Kaufman says.
Kaufman’s group has countered by engineering NK cells into better cancer fighters. “We can engineer these NK cells to provide additional mechanisms or more activated cells that seem to be able to overcome those barriers.”
They have done this by knocking out a gene called CISH, which is involved in regulating cell-signalling molecules called cytokines. NK cells without the CISH gene are more sensitive to the cytokine IL-15, which leads to greater cell proliferation. As a result, the cells live longer inside the body and show enhanced anti-tumour activity.2
Trials ahead
Several challenges remain. Like CAR-T cells, NK cell therapies seem less effective against solid tumours. And because they are not based on host cells, the engineered NK cells can trigger an immune response, which tries to reject them. Researchers deal with that at present with doses of chemotherapy to suppress the host immune system. But Kaufman says they are also working on a new type of “stealth” NK cell that can evade host immunity.
“Can you also engineer these cells to avoid that immune response? That’s a challenge for later,” he says.
Shoreline has completed preclinical testing on a potential NK cell therapy for acute myeloid leukaemia. The company is now working on ways to manufacture the cells to the required clinical grade, and to test them for safety. That work is on track, Kaufman says, and trials will begin soon.
Explore the anticancer potential of engineered natural killer cells here.
References
- 1.
Liu, S. et al. J. Hematol Oncol 14, 7 (2021)
- 2.
Zhu, H. et al. Cell Stem Cell 27, 224–237 (2020)
Intelligent Cells: Shoreline Builds Immunotherapy Platform, Pipeline with $140M Financing
Shoreline Biosciences has developed induced pluripotent stem cell (iPSC)-derived natural killer (NK) cells and macrophages that are optimized by applying gene editing to target specific genes with properties sought by the company. San Diego-based Shoreline says its “intelligently engineered” NK cells can target and kill tumors more effectively and efficiently…
[Full article text: https://www.genengnews.com/topics/drug-discovery/intelligent-cells-shoreline-builds-immunotherapy-platform-pipeline-with-140m-financing]
California Life Sciences awarded Kite Pharma, a Gilead company, and Shoreline Biosciences the 2021 Strategic Partnership of the Year Award
Shoreline Biosciences, Inc. is thrilled and honored to be recognized by the California Life Sciences (CLS) as the #Pantheon2021 award winner for the Strategic Partnership of the Year Award. Thank you, Kite Pharma, a Gilead company; we are incredibly grateful for your continued partnership as we develop safe, effective, and affordable iPSC-derived cell therapies.
Watch the full video here: https://bit.ly/3mNQTUA
Developing Allogeneic Induced Pluripotent Stem Cell Based Therapies to Kill Cancer Cells with Kleanthis Xanthopoulos Shoreline Biosciences
Nov 4, 2021
Kleanthis Xanthopoulos is Co-Founder and CEO of Shoreline Biosciences. He talks about the Shoreline cell therapy platform that uses standardized manufacturing of allogeneic induced pluripotent stem cells to create an effective treatment to kill tumor cells with multiple advantages over autologous T-cell therapies.
Kleanthis explains, “We are focusing specifically on two different effector cells, Natural Killers and Macrophages, and we derive them from a platform which is induced pluripotent stem cells. This gives us the ability to really engineer the NK cells and Macrophages that we derive from iPSC, so they become allogeneic standardized, meaning they can be introduced to any patient and then are targeted and specific.”
“Initial clinical results are showing us that iPSC derived NK cells don’t appear to have the kind of side effects that you see with T-cells. So we are very, very excited about that. And we are seeing that there’s a different dimension in cell therapies that can be served very, very nicely through these allogeneic pluripotent stem cell based therapies.”
After the interview, Shoreline announced it has raised $140 million in its latest fundraising round.
#ShorelineBio #ShoreBiosciences #Oncology #Immunotherapy #NKCells #iPSC #Macrophages #SanDiego
Shoreline Biosciences – (iPSC)-Derived Allogeneic Natural Killer (NK) and Macrophage Products
Dr. Kleanthis Xanthopoulos, co-founder, Chairman and CEO of Shoreline Biosciences, discusses the development of genetically engineered induced pluripotent stem cell (iPSC)-derived allogeneic natural killer (NK) and macrophage products that are intelligently designed for greater specificity, potency and persistence, overcoming the limitations of early cell therapies, for use in oncology and regenerative medicine.
Kleanthis is a serial biotechnology entrepreneur with over two decades of experience in the biotechnology and pharmaceutical research industries as an executive, company founder, chief executive officer, investor and board member.
Dr. Xanthopoulos has founded five companies, introduced three life science companies to NASDAQ and financed and brokered numerous creative strategic alliance and partnership deals with large pharmaceutical partners.In addition to his role at Shoreline Biosciences, Dr. Xanthopoulos is the Chairman of Stork Capital Life Sciences which focuses on building and investing in innovative biotechnology companies. Dr. Xanthopoulos is a member of the board of directors of IRRAS AB, Connect Biopharma, (NASDAQ: CNTB), Zosano Pharma, Inc., (NASDAQ: ZSAN), and is the co-founder and a member of the board of directors of privately held Sente Inc.
Previously, he served on the boards of LDO sp.a. (Milan, Italy), Odyssey Therapeutics, Anadys Pharmaceuticals and Regulus Therapeutics.
Dr. Xanthopoulos participated in The Human Genome Project as a Section Head of the National Human Genome Research Institute from 1995 to 1997. Prior to this, he was an Associate Professor at the Karolinska Institute, Stockholm, Sweden. An Onassis Foundation scholar, Dr. Xanthopoulos received his B.Sc. in Biology with honors from Aristotle University of Thessaloniki, Greece, and received both his M.Sc. in Microbiology and Ph.D. in Molecular Biology from the University of Stockholm, Sweden.
https://healthprofessionalradio.com.au/shoreline-biosciences-ipsc-derived-allogeneic-natural-killer-nk-and-macrophage-products/
Fresh off Kite and BeiGene deals, Shoreline ups the ante with a hefty crossover
Editor: Max Gelman
Though it may seem like Shoreline Biosciences is rapidly gaining momentum with a flurry of deals — and, now, a new funding round — Kleanthis Xanthopoulos doesn’t feel he’s in a rush.
The biotech’s chief executive put the bow on a $140 million Series B on Tuesday, as Shoreline continues a streak of wheeling and dealing that’s seen it partner with Gilead’s Kite and BeiGene these last few months. And despite the new raise technically being a crossover round with Ally Bridge Group leading the way, Xanthopoulos is taking his time in prepping a public offering.
“It’s only smart for us to be ready for an IPO, but we have so much capital we can pick the right timing,” Xanthopoulos told Endpoints News. “Practically, we’re going to be ready to become a public company. When the time comes, we’ll be set, but it’s good to have that luxury.”
Driving all the interest are Shoreline’s off-the-shelf cancer therapies, including a particular focus on iPSC NK cells and macrophages for various tumors. Partnered with Dan Kaufman’s lab out of UC-San Diego, Shoreline has built a war chest of $300 million to advance such treatments, build out its manufacturing capabilities and sign its high-profile collaborations.
Manufacturing specifically has a special place in Shoreline’s plans, as Xanthopoulos eventually hopes the company will be able to create NK cell therapies that will be used in the community setting. It’s a pitch that’s driven significant investment toward the field as a whole, with companies like Artiva gaining backing from blue-chip investors and Merck.
But Shoreline’s focus on pluripotent stem cells — compared to Artiva’s donor cell approach — gives it a key differentiating factor, Xanthopoulos said. The two have very different manufacturing processes and the CEO believes iPSC NK cells will prove safer and more cost-effective in the long run.
“We incorporated AI, automation to completely rethink how we’re going to create the manufacturing,” he said. “We’ve recruited people from the electronic chip manufacturing industry to see how it worked there. A large portion of the raise is earmarked to build that facility.”
The company is now sitting on 10 pipeline programs largely aimed at a variety of hematological and solid tumors. Xanthopoulos said there are nine candidates involving NK cells, including two in house, three from the Kite partnership and four being co-developed with BeiGene. The last is Shoreline’s in-house macrophage program, which is slightly behind the rest, the CEO said.
Xanthopoulos likes to think of it as not just Shoreline’s pipeline, however, but the pipelines of three different companies coming together. Moving forward, Shoreline is getting ready to send its first IND for the lead in-house NK cell therapy by the end of 2022, with plans to submit “one or two” INDs every year after that, Xanthopoulos said.
And once that’s accomplished, maybe the IPO will come. But Xanthopoulos isn’t counting his cell therapies before they come home to roost.
“We want to see [our therapies] as broadly available as antibodies,” he said. “It should be that simple given how safe the NK cells have proven to be in the clinic.”
https://endpts.com/fresh-off-kite-and-beigene-deals-shoreline-ups-the-ante-with-a-hefty-crossover-but-the-biotech-insists-its-in-no-rush/